Postpartum is the term used to refer to the time after childbirth. Whilst early literature refer to this period as the first six weeks after birth, the World Health Organisation (WHO) describe it as the period that begins immediately after childbirth and until the mother’s hormone level and uterus size returns to a non-pregnant state, usually a period of up to six months. The WHO defines this postnatal period as ‘the most critical and yet most neglected phase in the lives of mothers and babies.’
Physical changes and emotional responses
For most women, the postpartum period heralds many physical changes that can be accompanied by a variety of emotional responses. This is because immediately after childbirth, there is a dramatic drop in both oestrogen and progesterone hormonal levels in the body whilst both prolactin and oxytocin levels, hormones that help in breastfeeding fluctuate throughout the day. It is also an acutely stressful period adjusting to motherhood and changes within a partnership, dealing with pain and soreness post-delivery, tackling breastfeeding, dealing with sleep changes and deprivation as well as reacting to the experience of childbirth itself.
What are the ‘baby blues’ and how do I manage them?
Between 50%-80% mothers get the ‘baby blues’, lasting up to two weeks after the baby is born. The ‘baby blues’ often start around 3 days from birth and are seen as an obvious, short-term result of adjustment to falling hormonal levels, which pass as hormones start to rise on day four. Some features of the ‘baby blues’ include being emotional or tearful, irritable, or touchy, a rise in anxiety and low mood.
Ask for help
It’s easy to feel overwhelmed and exhausted when experiencing the ‘Baby Blues’, so try asking another caring adult to be with you until they pass (usually 4-7 days post the baby). Ask friends and family to bring your meals and help with any important chores. Get help in caring for your other children.
Lower your expectations
Try and sleep as and when you can and change any high expectations you have of what you want to do at this time, and this includes avoiding putting yourself under pressure to create an emotional bond with your baby. Keep in mind that you will naturally develop this bond by being close and together.
Make a list of some things you usually do to care for yourself, such as rubbing on some nice hand cream, having a bath, putting on some make-up, and so on. Make sure you work your way through the list. Most of all, remind yourself that the feelings will pass and that you can’t speed the process of hormone balance and they will naturally work themselves out.
What is postnatal or postpartum depression (PND)?
Around 1 in 10 women are affected by postpartum or postnatal depression. This condition usually starts within a year of giving birth and for a diagnosis, lasts at least two weeks. A diagnosis of PND should be made by a mental health professional, but some signs include:
Symptoms of postnatal depression
Not being able to enjoy anything, persistent feelings of sadness and low mood, hopelessness, not being able to stop crying, feelings of not being able to cope, difficulty sleeping, loss of interest in the baby, extreme tiredness, extreme anxiety, panic attacks, loss of appetite, neglect of self-care, uncontrollable bouts of anger, lack of interest in sex, feelings of worthlessness and intense guilt. Very occasionally there may be frightening thoughts, such as hurting yourself and/or hurting your baby.
There are many effective treatments that help with PND and early diagnosis and treatment will get you back on track. Some women worry about seeking help since they think it might indicate a sign of their inability to look after the baby. This is absolutely not the case, since PND is recognised as an ill-health condition requiring prompt and effective treatment.
Is Partner or Paternal PND (PPD) a real condition?
The postpartum periods with its many adjustments pose risks for depression for partners. Estimates of PPD in the first two months postpartum vary from 4-25% and generally correlates with maternal PND. Some symptoms may include unworthiness, sadness, anxiety, prolonged lowering of mood and lethargy, avoidance of adjusting to having a baby through overworking, drinking and substance abuse, frustration, irritability, getting into fights, not doing well at work, reduced interest in sex, socialising less.
What makes someone more vulnerable to either PND or PPD?
There are many contributors to PND both biological and psychosocial, but the most significant is antenatal or prenatal mental health since almost a third of postnatal depression begins in pregnancy or pre-pregnancy. There may be a higher risk if there is a history or familial history of anxiety or depression, a poor relationship with a partner, a stressful experience of conception or difficult pregnancy, physical conditions such as, for example, underactive thyroid or a chronic illness.
In terms of risk factors for partners, the same factors as for mothers apply, triggered by the pressure of new responsibilities, money worries, work stress, relationship with other children and the impact of the birth experience.
What can I do to help manage PND or PPD?
- Tell someone, break the secrecy
- Make a plan to self-care by taking small steps to talk, be active, eat well, get help with sleep and every time you achieve a goal acknowledge and reward yourself
- Keep a mood and thought diary – useful to take to the doctor’s and to recognise and manage self-defeating thoughts and actions
- Access psychological help, early intervention works.
- Antidepressants may help and those prescribed will be safe whilst breastfeeding
- Peer/group support
How much does the birth experience impact postpartum recovery? Postnatal Traumatic Stress Disorder
In my opinion, the traumatic impact of a complicated or traumatic birth experience is underestimated. This trauma may be related to the birth experience itself but will be magnified if there are past experiences of trauma, including childhood trauma, sexual trauma, traumatic loss and previous birth associated trauma. Whilst the presentation of postnatal trauma may be as depression, it is important to address the trauma experience in psychological treatment. In this instance, there are targeted trauma-focused interventions that should be offered to firstly the mother, but also to the partner.
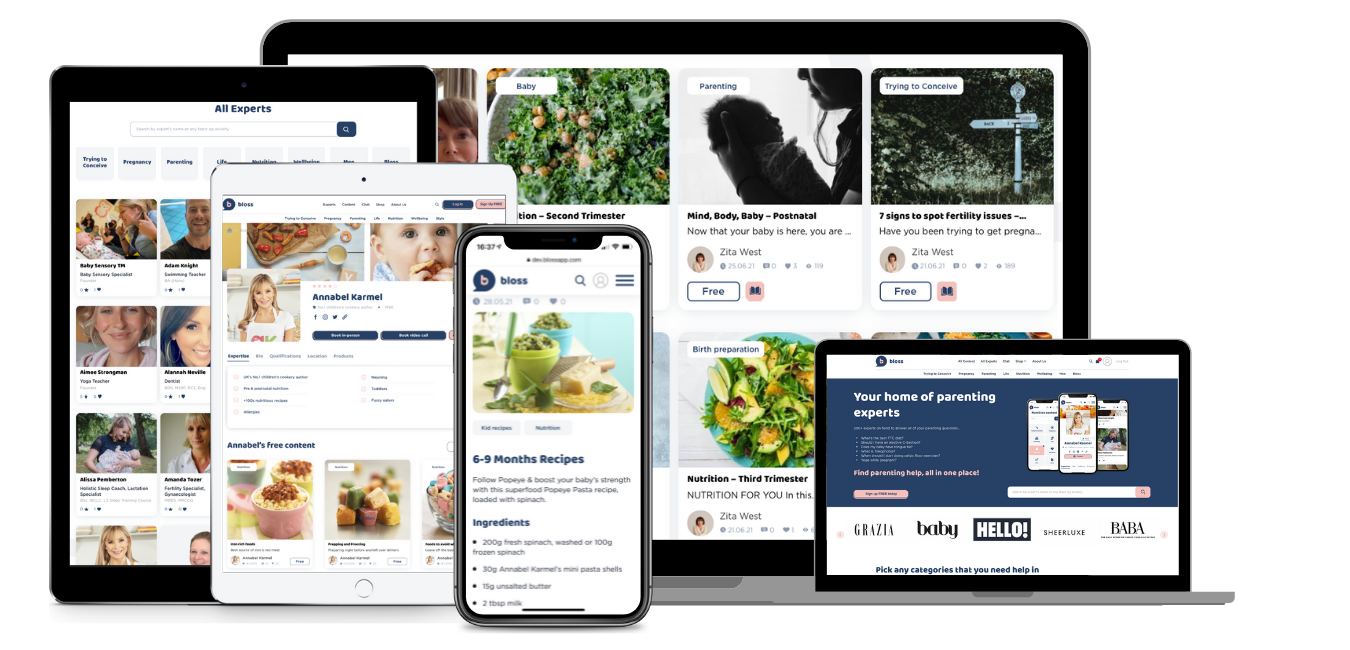
Sign up today for unlimited access:
- Book appointments
- Expert advice & tips
- Premium videos & audio
- Curated parenting newsletters
- Chat with your bloss community
- Discounts & competitions
- Special events




Leave a Comment
You must be logged in to post a comment.